Preparing and certifying the family physicians that Canada needs
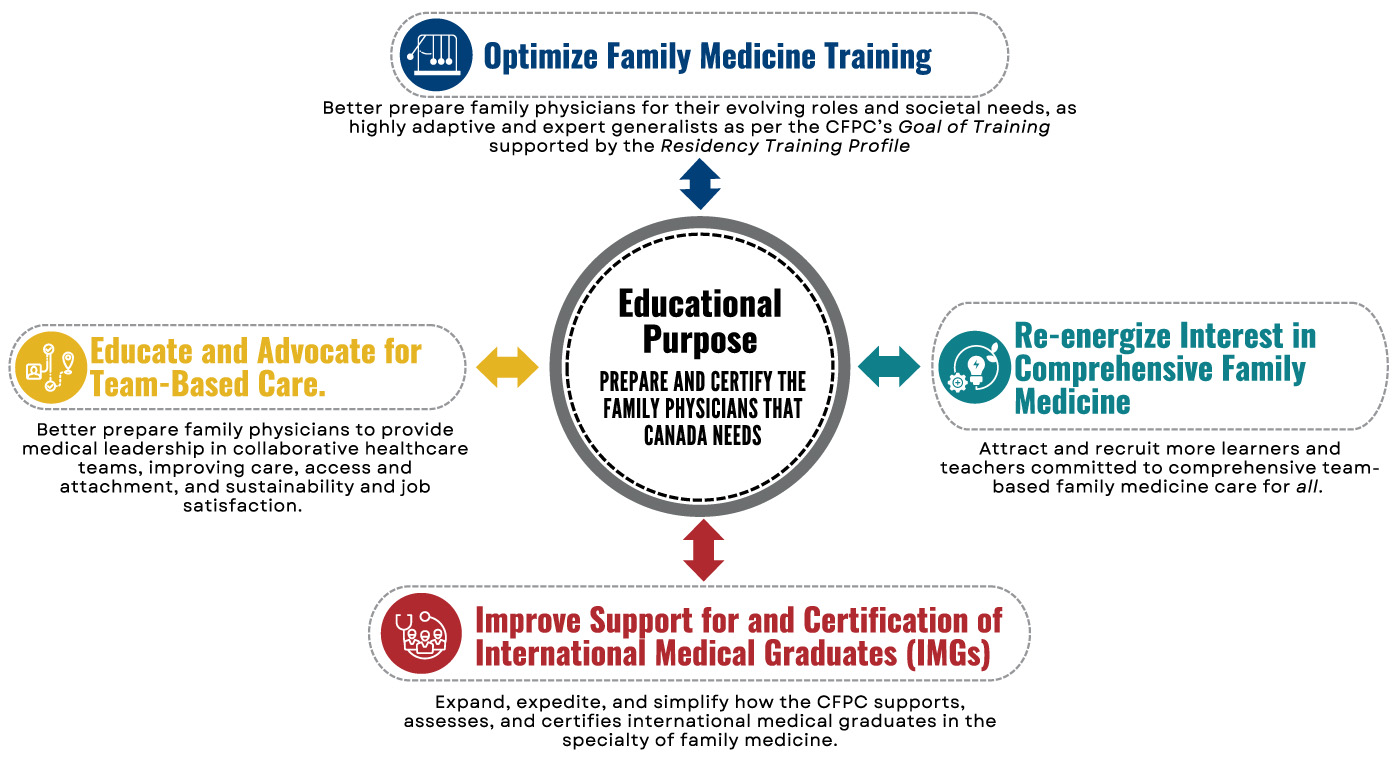 In response to the current health system crisis with an extreme shortage of family physicians, and based on consultation with our educational community, the College of Family Physicians of Canada (CFPC) has developed an Educational Action Plan (EAP) based on four educational priorities.
In response to the current health system crisis with an extreme shortage of family physicians, and based on consultation with our educational community, the College of Family Physicians of Canada (CFPC) has developed an Educational Action Plan (EAP) based on four educational priorities.The EAP will guide educational activities at the CFPC and is designed in the spirit of continuous improvement and social accountability with a plan to evaluate residency program and health system outcomes and influences which will inform future iterations.
Read more about the Educational Action Plan
The CFPC is stepping up to help solve the family physician recruitment, retention and capacity needs in Canada. Education matters!
The CFPC is the educational standard setting and certifying body for family medicine representing over 45,000 members. We support family medicine teaching and research and advocate on behalf of the specialty of family medicine, family physicians, and the patients they serve.
Through these roles, we help to shape the health workforce. The EAP is centred on our purpose to prepare and certify the family physicians that Canada needs in support of the Quintuple Aim to improve patient experience, population health, provider well-being, value, and health equity.
The need is great to improve the number, mix, distribution and capacity of family physicians in Canada and governments have expanded and opened new medical schools with the aim of addressing the shortage. But increased positions alone will not guarantee more family physicians. The CFPC seeks to work with its academic partners to improve the success of these initiatives.
 We can’t do it alone!
We can’t do it alone!
We will engage with CFPC members and committees, universities, medical organizations, regulators, governments and patient partners in several key educational activities aimed at improving recruitment, retention and capacity of family physicians working in Canada.
